Understanding the menstrual cycle
- Mar 25, 2024
- 4 min read

Ah, it comes that time of the month again, when mood fluctuates, and cramps make life unbearable. I’m of course talking about the monthly “period” that most women experience throughout their adulthood. Despite being a common phenomenon among girls and women, there are still many individuals out there who do not know what this monthly “period” is and how it actually affects the physiology of women. Hence, this article aims to unravel some of the mysteries behind this monthly visitor and bust some myths regarding it too.
First of all, let’s introduce some terms that we will be using later on. This monthly period is known as the menstrual cycle and usually occurs every 28 days or so. The biology behind this cycle mainly involves the hypothalamus, a part of our brain that controls a lot of homeostatic mechanisms, the pituitary gland, a gland right below the hypothalamus, the ovaries, and the endometrium, the inner lining of a woman’s uterus.

Figure 1: Organs involved in the menstrual cycle. The green part is the hypothalamus, while the red part is the pituitary gland.
As the menstrual cycle is well a cycle, it does not matter where we start, as we will eventually end up at the same phase. Therefore, we define day 0, or the start of menses, as the first day of menstrual bleeding. This happens due to low levels of progesterone and estrogen, causing the endometrium to shed. A few days before this, a structure known as the corpus luteum, which we will discuss later, starts to degenerate. This results in low levels of the hormones inhibin A, estrogen, and progesterone. Together, these stimulate the hypothalamus to secrete gonadotropin-releasing hormone (GnRH) that acts on the anterior pituitary gland to cause the release of follicle-stimulating hormone (FSH) and luteinizing hormone (LH). This elevation in FSH is responsible for recruiting primordial follicles in the ovary to grow, and eventually select for one dominant follicle. An ovarian follicle consists of a group of granulosa cells, and theca cells, surrounding an oocyte which eventually matures into a fertilizable cell.
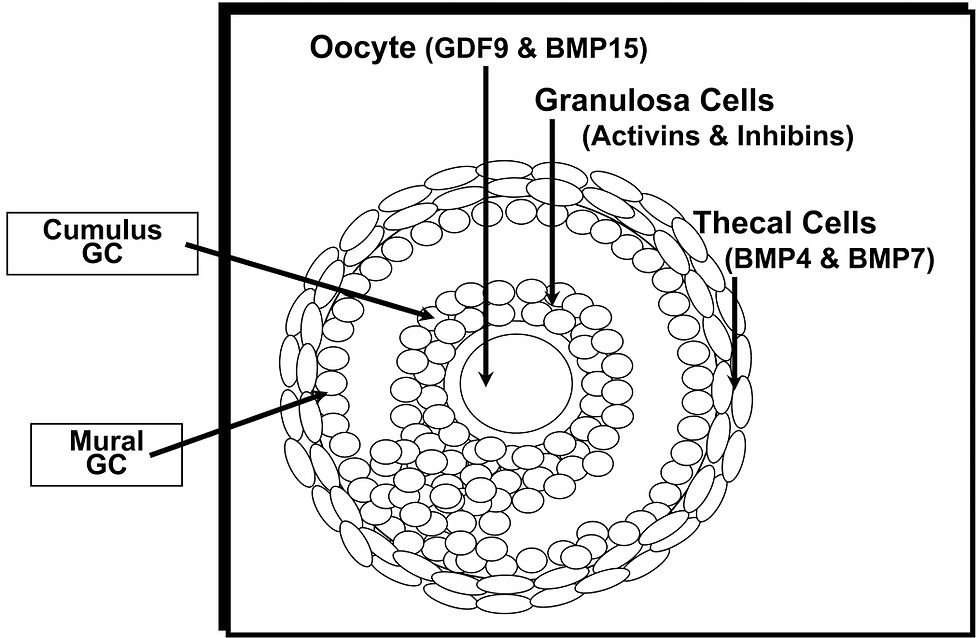
Figure 2: Anatomy of an ovarian follicle. Image taken from “Menstrual Cycle: Basic Biology” (Hawkins and Matzuk, 2008).
After recruitment, these follicles grow into primary and secondary follicles. FSH stimulates the proliferation of granulosa cells on the follicles which synergize with the theca cell to produce estrogen, which acts on the anterior pituitary to decrease FSH release in a negative feedback mechanism. As a result, growing follicles that are not as developed as the dominant follicle lose their ability to produce estrogen and eventually degenerate.
As the dominant follicle continues to develop, it produces more estrogen. Estrogen causes the endometrium to thicken and become more vascular (filled with blood vessels). After crossing a certain threshold, estrogen also stimulates the anterior pituitary to produce high amounts of LH. This causes the LH surge that increases prostaglandins and proteolytic enzyme levels. These enzymes digest collagen in the follicular wall and cause the oocyte to be released from the ovary. This process is known as ovulation and involves cyclooxygenase enzymes to produce the prostaglandins. Hence, non-steroidal anti-inflammatories drugs (NSAIDs) such as ibuprofen are often contraindicated for patients with infertility as it could prevent ovulation.

Figure 3: Stages of ovarian follicle development. Image taken from “Menstrual Cycle: Basic Biology” (Hawkins and Matzuk, 2008).
After ovulation, the follicles that once “house” the oocytes become the corpus luteum which produces the hormone inhibin A, and suppresses FSH production. The corpus luteum also produces the hormone progesterone that helps maintain the thickness of the endometrium and makes it receptive to a fertilized embryo.

Figure 4: Diagram of the menstrual cycle. Image taken from Wikipedia.
The cycle can now go in two directions. If the oocyte is fertilized by a sperm, an embryo will be formed that stimulates the placenta to release a hormone known as human chorionic gonadotropin (hCG), which maintains the corpus luteum and hence the endometrium. If fertilization does not occur, the corpus luteum degenerates, reducing inhibin A, progesterone, and estrogen levels. This causes the blood vessels in the endometrium to vasoconstrict and shed, and the cycle begins again.
Myth 1: You can’t exercise during menses
This is one myth that I truly despise as it discourages women from doing physical activity without a concrete basis. In fact, exercising has been shown to reduce many side effects of menstruation such as premenstrual syndrome (PMS) symptoms, and period pain, as well as improve energy levels.
Myth 2: PMS is just a mental condition
PMS is a combination of symptoms associated with menstruation, and it causes symptoms such as irritability, fatigue, anxiety, or feelings of sadness before or during menstruation. Although the exact cause has not been pinpointed, fluctuation of hormone levels during menstruation seems to play a role, as women with PMS are hypersensitive to these changes compared to women without PMS.
Myth 3: Cold food should be avoided during menstruation
Ultimately, there is scarce research examining the effects of “cold” food specifically affecting period cramps. The reason some may associate “cold” food with worsening period cramps may be that most “cold” foods such as ice cream are processed, and may increase inflammation, though that itself has not yet been proven yet. As such, there is no need to actively avoid cold food or drinks during period cramps, unless you believe they hurt you, which may exaggerate the nocebo effect.
Conclusion
An average woman experiences menstruation for a total of 7 years in their lifetime. Hence, understanding the biology of menstrual cycles is definitely beneficial for regulating activities, mood, and many other aspects in life; and for the boys out there, understanding it may come in handy some time for your loved ones.
Article prepared by: Jared Ong Kang Jie, Research and Development Director of MBIOS 23/24
If you enjoyed this article, do sign up to become a part of our MBIOS family and receive our monthly newsletter along with many more resources in the link below.
References
Hawkins, S.M. and Matzuk, M.M. (2008). The Menstrual Cycle. Annals of the New York Academy of Sciences, 1135(1), pp.10–18. doi:https://doi.org/10.1196/annals.1429.018.
Nworie, K.M. (2018). Premenstrual syndrome: etiology, diagnosis and treatment. A mini literature review. Journal of Obstetrics and Gynecological Investigations, 1(1), pp.41–46. doi:https://doi.org/10.5114/jogi.2018.78010.
Reed, B.G. and Carr, B.R. (2018). The Normal Menstrual Cycle and the Control of Ovulation. [online] Nih.gov. Available at: https://www.ncbi.nlm.nih.gov/books/NBK279054/.
Sanchez, B.N., Kraemer, W.J. and Maresh, C.M. (2023). Premenstrual Syndrome and Exercise: A Narrative Review. Women, [online] 3(2), pp.348–364. doi:https://doi.org/10.3390/women3020026.
Thiyagarajan, D.K., Basit, H. and Jeanmonod, R. (2019). Physiology, menstrual cycle. [online] National library of medicine. Available at: https://www.ncbi.nlm.nih.gov/books/NBK500020/.

Comments